Abstract
Background: Achievement of initial remission remains the most important clinical factor predicting long term survival in acute myeloid leukemia (AML) patients treated with intensive chemotherapy. Yet, whether the patient subset in need of a second cycle of intensive induction chemotherapy to reach remission experiences inferior outcomes compared to patients reaching remission after a single cycle of therapy, remains uncertain with previous publication showing diverging outcomes with respect to patient survival and the risk for disease relapse (Rowe et al. Cancer 2010; Othus et al. Leukemia 2016). In this analysis we aimed to readdress this important clinical question in a uniform cohort of recently treated patients.
Patients and Methods: Retrospective analysis of 302 consecutive AML patients treated with intensive induction chemotherapy in our institution in 2007-2020. Univariate analyses were performed using T-Test for continuous variables, and Fisher's Exact test and Pearson's chi-squared for assessment of categorical variables. Overall survival was assessed using the Kaplan-Meier method, and the log-rank test was used to compare overall survival between groups. Multivariate analyses using logistic regression were performed using year of diagnosis, patient age, follow-up duration, patient gender, white blood cell (WBC) count at diagnosis, MRC cytogenetic risk category, FMS-like tyrosine kinase-3 internal tandem duplication (FLT3-ITD) and nucleophosmin 1 (NPM1) status, and ELN 2017 risk category, as covariates. All tests were two-sided with the type I error rate set at 0.05 for the determination of factors associated with time-to-event outcomes.
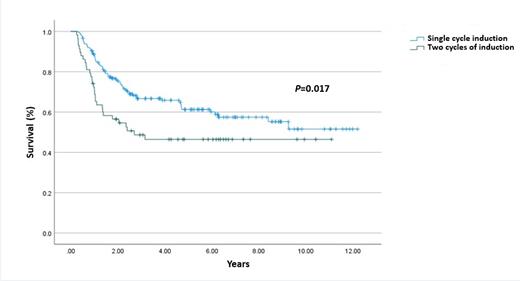
Results: Median patient age was 55 years with a median follow-up duration of 23 months. In terms of European LeukemiaNet (ELN) 2017 classification, 122 patients (40%) were designated as favorable risk disease, 108 patients (36%) were intermediate risk, and 71 patients (24%) were adverse risk. A hundred and seventy-seven patients (60%) attained remission following initial chemotherapy while 58 patients (20%) required an additional cycle of intensive chemotherapy for remission. Patients requiring two cycles to reach remission were less likely to be NPM1 mutated (33% versus 51%; p=0.025) or be in the ELN 2017 favorable risk category (25% versus 57%; p<0.001). In multivariate analysis achievement of remission following 2 cycles of intensive compared with a single cycle resulted in significantly inferior survival [hazard ratio (HR)=1.68, 95% CI, 1.09-2.59; p=0.017] (figure 1) whereas leukemia-free survival was not significantly impacted (HR=1.26, 95% CI, 0.85-1.85) (p=0.23). Relapse rates also did not differ to a significant degree between groups (45% versus 47%, p=0.8).
Conclusion: Our analysis reaffirms the indispensable clinical significance of attainment of an early remission following intensive induction chemotherapy for AML patients. The marked long term survival advantage conferred by an early remission speaks to the need to improve initial remission rates which with the recent introduction of novel targeted therapeutics seems to be an attainable goal.
Avigdor: Gilead: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; BMS: Research Funding; Janssen: Research Funding; Takeda: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal